Chronic wounds the global problem
187 million people worldwide have wounds either as a result of surgery, trauma or burns. Wound healing can be delayed as a result of patient comorbidities such as diabetes or venous disease. 21% of all wounds are chronic and the problem is growing.1 Venous Leg Ulcers, Diabetic Foot Ulcers and Pressure Ulcers are complex wounds that require early treatment to prevent them from becoming chronic. The common challenges in wound care and their impact on patients were identified by a panel of experts.2
“Delayed referral can put patients’ limbs and lives at risk.”
“It is a concern when patients are seen by the same clinician week on week when the wound is not progressing, or worse, is deteriorating, and the patient is not referred to a specialist.”
“The personal cost of an amputation for the patient is huge – it can be challenging adjusting to life after losing a limb and there may be a need for home environments to be adapted to make it more accessible.”
“Patients with infected wounds can experience pain, swelling, increased exudate and odour. It is important for patients to receive appropriate care to stop the infection becoming systemic and leading to more severe complications, such as sepsis.”
“Prolonged inflammation can cause wounds to become stalled, and may result in increased scarring or chronic wounds. It is important for clinicians to identify and manage local and systemic factors.”
“Chronic wounds can ultimately have a devastating effect on the lives of patients and their close family. Staff caring for patients with non-healing wounds can become demoralised and may inappropriately label patients as non-concordant.”
References:
1. MedMarket Diligence Report 2013 2. Fletcher J., Luxmi D., Chadwick P., Checkley C., Dowsett C., Acton C., Stang D., Use of oxidised regenerated cellulose (ORC) and collagen dressings (PROMOGRAN™ Protease Modulating Matrix and PROMOGRAN PRISMA™ Wound Balancing Matrix) to kick-start the treatment of chronic wounds, Wounds UK 2020;1(16)
To overcome the challenges in wound care, the first principles of care, defined by the expert panel1, should be addressed.
Thorough holistic assessment of the patient and wound drives individualised patient care. Appropriate onward referral as per local protocol indicates good clinical knowledge and self-awareness.
A good patient–clinician relationship enables provision of consistent delivery of care as the patient moves through services. Maintaining clear communication with patients is important so they feel supported to self care and are confident in their care provider.
Selecting the most appropriate dressing to manage the symptom requires a good understanding of the disease aetiology and the dressing mode of action.
Pathways are an effective tool in standardising care, establishing safe practice and assisting healthcare professionals with decision-making.
Fletcher J., Luxmi D., Chadwick P., Checkley C., Dowsett C., Acton C., Stang D., Use of oxidised regenerated cellulose (ORC) and collagen dressings (PROMOGRAN™ Protease Modulating Matrix and PROMOGRAN PRISMA™ Wound Balancing Matrix) to kick-start the treatment of chronic wounds, Wounds UK 2020;1(16)

Wounds that do not progress beyond the inflammatory phase often demonstrate1:
It is well established that healing can only be achieved when the right amount of proteases are in the right place and for the right duration, in order to promote granulation tissue formation and stimulate wound healing.
Once holistic assessment and best practice have been carried out and infection has been excluded, it is important for clinicians to consider why the wound is still failing to progress to healing and if excess host proteases, such as MMPs and elastase, are the underlying cause.
Use of PROMOGRAN™ Matrix and PROMOGRAN PRISMA™ Matrix is beneficial in managing the underlying biochemistry of chronic wounds.
Educational support should be provided to healthcare professionals before the introduction of these dressings and for their use to be monitored in practice and outcomes of care measured.
The new proposed pathway for use in practice will help clinicians to identify a clear stop point of when these dressings should no longer be used, when to consider referral and when to re-assess and review the diagnosis, patient objectives and expectations.
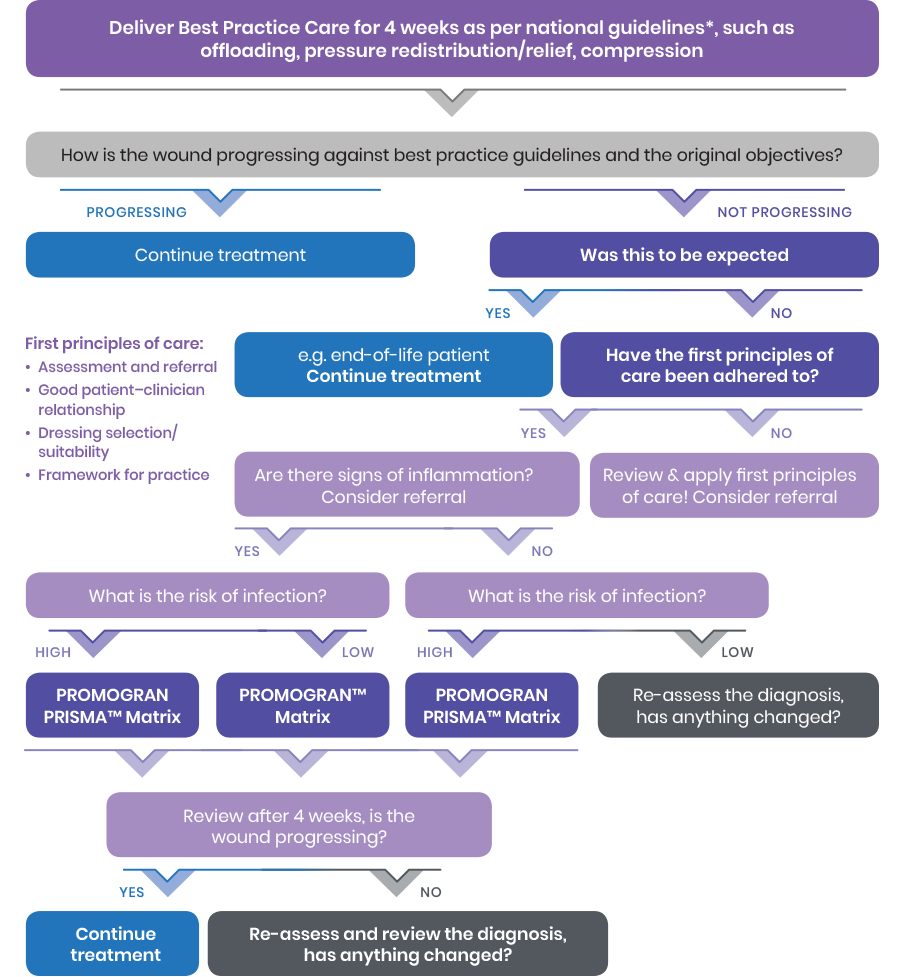
*e.g. NICE (2014) Pressure ulcers: prevention and management; NICE (2015) Diabetic foot problems: prevention and management; NICE (2017) Clinical Knowledge Summaries: Leg Ulcer – Venous; SIGN (2010) Management of chronic venous leg ulcers.” is also missing
References:
1. Fletcher J., Luxmi D., Chadwick P., Checkley C., Dowsett C., Acton C., Stang D., Use of oxidised regenerated cellulose (ORC) and collagen dressings (PROMOGRAN™ Protease Modulating Matrix and PROMOGRAN PRISMA™ Wound Balancing Matrix) to kick-start the treatment of chronic wounds, Wounds UK 2020;1(16)
Evaluation of PROMOGRAN PRISMA™ Matrix in hard-to-heal chronic wounds
Luxmi Dhoonmoon, Hana Hassan and Colette Spoard, Central and North West London NHS Foundation Trust, November 2019
CASE STUDY 1
This was a 78-year-old female patient living alone with chronic mixed aetiology leg ulcers for more than 10 years. Other medical history included essential hypertension and macular degeneration. She had previously been able to carry out activities of daily living independently; however, due to pain, mobility had declined, and she had become housebound. Previous treatment had been carried out by a district nurse. The patient was referred to a tissue viability nurse as the wound was non-healing, despite standard practice for leg ulcer management being followed.
Initial assessment: The wound was static and showed no signs of progress for more than 4 weeks, although appropriate wound care had been implemented. Exudate levels and malodour were high, which was problematic to the patient as she could not sleep or eat. After full holistic assessment and Doppler, compression bandaging (after vascular review) was applied, despite mixed aetiology, as the patient had declined vascular intervention. PROMOGRAN PRISMA™ Matrix was used to dress the wound to stimulate healing, following discussion with the patient (Figure 3a).
Results: After 55 days of treatment that included PROMOGRAN PRISMA™ Matrix for 5 weeks, the wound had reduced in size and comprised 100% healthy granulation tissue. Pain had reduced and malodour was no longer present. Mobility had also improved, with no concerns reported by the patient (Figure 3b).
After 5 months, the wound had healed (Figure 3c). The use of PROMOGRAN PRISMA™ Matrix encouraged wound healing, and the patient was able to return to her daily activities.

References:
1. Fletcher J., Luxmi D., Chadwick P., Checkley C., Dowsett C., Acton C., Stang D., Use of oxidised regenerated cellulose (ORC) and collagen dressings (PROMOGRAN™ Protease Modulating Matrix and PROMOGRAN PRISMA™ Wound Balancing Matrix) to kick-start the treatment of chronic wounds, Wounds UK 2020;1(16)
CASE STUDY 2
This was a 94-year-old female with a venous leg ulcer, which had rapidly deteriorated after the death of her husband. The patient had been emotionally, psychologically and physically low and despite the wound previously healing, she had not managed hosiery well and the leg had deteriorated.
Initial assessment: After being re-assessed by the tissue viability nurse, tendon could be seen in the wound bed. The wound management regimen had previously included antimicrobials and hydrogel dressings to manage the wound bed. The district nursing team worked very closely with the tissue viability nurse to ensure adequate wound bed preparation and skin care. Despite the planned intervention, no improvement was observed and it was agreed, as a team, to start PROMOGRAN PRISMA™ Matrix immediately, following sharp debridement (Figure 4a). Treatment
also included a multi-layer compression bandage, as oedema was not well controlled with her hosiery. Pain, odour and exudate were the most inconvenient factors for the patient at this time.
Results: PROMOGRAN PRISMA™ Matrix contributed positively in speeding the wound healing process (Figure 4b), despite tendon being visible. Pain, exudate and odour were now also under better control (Figure 4c).

References:
1. Fletcher J., Luxmi D., Chadwick P., Checkley C., Dowsett C., Acton C., Stang D., Use of oxidised regenerated cellulose (ORC) and collagen dressings (PROMOGRAN™ Protease Modulating Matrix and PROMOGRAN PRISMA™ Wound Balancing Matrix) to kick-start the treatment of chronic wounds, Wounds UK 2020;1(16)